NEET MDS Lessons
Orthodontics
Myofunctional Appliances
- Myofunctional appliances are removable or fixed devices that aim to correct dental and skeletal discrepancies by promoting proper oral and facial muscle function. They are based on the principles of myofunctional therapy, which focuses on the relationship between muscle function and dental alignment.
-
Mechanism of Action:
- These appliances work by encouraging the correct positioning of the tongue, lips, and cheeks, which can help guide the growth of the jaws and the alignment of the teeth. They can also help in retraining oral muscle habits that may contribute to malocclusion, such as thumb sucking or mouth breathing.
Types of Myofunctional Appliances
-
Functional Appliances:
- Bionator: A removable appliance that encourages forward positioning of the mandible and helps in correcting Class II malocclusions.
- Frankel Appliance: A removable appliance that modifies the position of the dental arches and improves facial aesthetics by influencing muscle function.
- Activator: A functional appliance that promotes mandibular growth and corrects dental relationships by positioning the mandible forward.
-
Tongue Retainers:
- Devices designed to maintain the tongue in a specific position, often used to correct tongue thrusting habits that can lead to malocclusion.
-
Mouthguards:
- While primarily used for protection during sports, certain types of mouthguards can also be designed to promote proper tongue posture and prevent harmful oral habits.
-
Myobrace:
- A specific type of myofunctional appliance that is used to correct dental alignment and improve oral function by encouraging proper tongue posture and lip closure.
Indications for Use
- Malocclusions: Myofunctional appliances are often indicated for treating Class II and Class III malocclusions, as well as other dental alignment issues.
- Oral Habits: They can help in correcting harmful oral habits such as thumb sucking, tongue thrusting, and mouth breathing.
- Facial Growth Modification: These appliances can be used to influence the growth of the jaws in growing children, promoting a more favorable dental and facial relationship.
- Improving Oral Function: They can enhance functions such as chewing, swallowing, and speech by promoting proper muscle coordination.
Advantages of Myofunctional Appliances
- Non-Invasive: Myofunctional appliances are generally non-invasive and can be a more comfortable option for patients compared to fixed appliances.
- Promotes Natural Growth: They can guide the natural growth of the jaws and teeth, making them particularly effective in growing children.
- Improves Oral Function: By retraining oral muscle function, these appliances can enhance overall oral health and function.
- Aesthetic Appeal: Many myofunctional appliances are less noticeable than traditional braces, which can be more appealing to patients.
Limitations of Myofunctional Appliances
- Compliance Dependent: The effectiveness of myofunctional appliances relies heavily on patient compliance. Patients must wear the appliance as prescribed for optimal results.
- Limited Scope: While effective for certain types of malocclusions, myofunctional appliances may not be suitable for all cases, particularly those requiring significant tooth movement or surgical intervention.
- Adjustment Period: Patients may experience discomfort or difficulty adjusting to the appliance initially, which can affect compliance.
Catalan's Appliance
Catalan's appliance, also known as the Catalan appliance or lower inclined bite plane, is an orthodontic device primarily used to correct anterior crossbites and manage dental arch relationships. It is particularly effective in growing children and adolescents, as it helps to guide the development of the dental arches and improve occlusion.
Indications for Use
-
Anterior Crossbite:
- The primary indication for Catalan's appliance is to correct anterior crossbites, where the upper front teeth are positioned behind the lower front teeth when the jaws are closed.
-
Space Management:
- It can be used to create space in the dental arch, especially when there is crowding or insufficient space for the eruption of permanent teeth.
-
Guiding Eruption:
- The appliance helps guide the eruption of the permanent teeth into a more favorable position, promoting proper alignment.
-
Facilitating Growth:
- It can assist in the growth of the maxilla and mandible, helping to achieve a more balanced facial profile.
Design and Features
-
Components:
- The Catalan's appliance typically consists of:
- Acrylic Base: A custom-fitted acrylic base that covers the lower anterior teeth.
- Inclined Plane: An inclined plane is incorporated into the appliance, which helps to reposition the anterior teeth by providing a surface for the teeth to occlude against.
- Retention Mechanism: The appliance is retained in the mouth using clasps or other anchorage methods to ensure stability during treatment.
- The Catalan's appliance typically consists of:
-
Customization:
- The appliance is custom-made for each patient based on their specific dental anatomy and treatment needs. This ensures a proper fit and effective function.
Mechanism of Action
-
Correction of Crossbite:
- The inclined plane of the Catalan's appliance exerts forces on the anterior teeth, encouraging them to move into a more favorable position. This helps to correct the crossbite by allowing the maxillary incisors to move forward relative to the mandibular incisors.
-
Space Creation:
- By repositioning the anterior teeth, the appliance can create additional space in the dental arch, facilitating the eruption of permanent teeth and improving overall alignment.
-
Guiding Eruption:
- The appliance helps guide the eruption of the permanent teeth by maintaining proper arch form and preventing unwanted movements of the teeth.
Angle’s Classification of Malocclusion
Malocclusion refers to the misalignment or incorrect relationship between the teeth of the two dental arches when they come into contact as the jaws close. Understanding occlusion is essential for diagnosing and treating orthodontic issues.
Definitions
- Occlusion: The contact between the teeth in the mandibular arch and those in the maxillary arch during functional relations (Wheeler’s definition).
- Malocclusion: A condition characterized by a deflection from the normal relation of the teeth to other teeth in the same arch and/or to teeth in the opposing arch (Gardiner, White & Leighton).
Importance of Classification
Classifying malocclusion serves several purposes:
- Grouping of Orthodontic Problems: Helps in identifying and categorizing various orthodontic issues.
- Location of Problems: Aids in pinpointing specific areas that require treatment.
- Diagnosis and Treatment Planning: Facilitates the development of effective treatment strategies.
- Self-Communication: Provides a standardized language for orthodontists to discuss cases.
- Documentation: Useful for recording and tracking orthodontic problems.
- Epidemiological Studies: Assists in research and studies related to malocclusion prevalence.
- Assessment of Treatment Effects: Evaluates the effectiveness of orthodontic appliances.
Normal Occlusion
Molar Relationship
According to Angle, normal occlusion is defined by the relationship of the mesiobuccal cusp of the maxillary first molar aligning with the buccal groove of the mandibular first molar.
Angle’s Classification of Malocclusion
Edward Angle, known as the father of modern orthodontics, first published his classification in 1899. The classification is based on the relationship of the mesiobuccal cusp of the maxillary first molar to the buccal groove of the mandibular first molar. It is divided into three classes:
Class I Malocclusion (Neutrocclusion)
- Definition: Normal molar relationship is present, but there may be crowding, misalignment, rotations, cross-bites, and other irregularities.
- Characteristics:
- Molar relationship is normal.
- Teeth may be crowded or rotated.
- Other alignment irregularities may be present.
Class II Malocclusion (Distocclusion)
- Definition: The lower molar is positioned distal to the upper molar.
- Characteristics:
- Often results in a retrognathic facial profile.
- Increased overjet and overbite.
- The mesiobuccal cusp of the maxillary first molar occludes anterior to the buccal groove of the mandibular first molar.
Subdivisions of Class II Malocclusion:
- Class II Division 1:
- Class II molars with normally inclined or proclined maxillary central incisors.
- Class II Division 2:
- Class II molars with retroclined maxillary central incisors.
Class III Malocclusion (Mesiocclusion)
- Definition: The lower molar is positioned mesial to the upper molar.
- Characteristics:
- Often results in a prognathic facial profile.
- Anterior crossbite and negative overjet (underbite).
- The mesiobuccal cusp of the upper first molar falls posterior to the buccal groove of the lower first molar.
Advantages of Angle’s Classification
- Comprehensive: It is the first comprehensive classification and is widely accepted in the field of orthodontics.
- Simplicity: The classification is straightforward and easy to use.
- Popularity: It is the most popular classification system among orthodontists.
- Effective Communication: Facilitates clear communication regarding malocclusion.
Disadvantages of Angle’s Classification
- Limited Plane Consideration: It primarily considers malocclusion in the anteroposterior plane, neglecting transverse and vertical dimensions.
- Fixed Reference Point: The first molar is considered a fixed point, which may not be applicable in all cases.
- Not Applicable for Deciduous Dentition: The classification does not effectively address malocclusion in children with primary teeth.
- Lack of Distinction: It does not differentiate between skeletal and dental malocclusion.
Tongue Thrust
Tongue thrust is characterized by the forward movement of the tongue tip between the teeth to meet the lower lip during swallowing and speech, resulting in an interdental position of the tongue (Tulley, 1969). This habit can lead to various dental and orthodontic issues, particularly malocclusions such as anterior open bite.
Etiology of Tongue Thrust
-
Retained Infantile Swallow:
- The tongue does not drop back as it should after the eruption of incisors, continuing to thrust forward during swallowing.
-
Upper Respiratory Tract Infection:
- Conditions such as mouth breathing and allergies can contribute to tongue thrusting behavior.
-
Neurological Disturbances:
- Issues such as hyposensitivity of the palate or disruption of sensory control and coordination during swallowing can lead to tongue thrust.
-
Feeding Practices:
- Bottle feeding is more likely to contribute to the development of tongue thrust compared to breastfeeding.
-
Induced by Other Oral Habits:
- Habits like thumb sucking or finger sucking can create malocclusions (e.g., anterior open bite), leading to the tongue protruding between the anterior teeth during swallowing.
-
Hereditary Factors:
- A family history of tongue thrusting or related oral habits may contribute to the development of the condition.
-
Tongue Size:
- Conditions such as macroglossia (enlarged tongue) can predispose individuals to tongue thrusting.
Clinical Features
Extraoral
- Lip Posture: Increased lip separation both at rest and during function.
- Mandibular Movement: The path of mandibular movement is upward and backward, with the tongue moving forward.
- Speech: Articulation problems, particularly with sounds such as /s/, /n/, /t/, /d/, /l/, /th/, /z/, and /v/.
- Facial Form: Increased anterior facial height may be observed.
Intraoral
- Tongue Posture: The tongue tip is lower at rest due to the presence of an anterior open bite.
- Malocclusion:
- Maxilla:
- Proclination of maxillary anterior teeth.
- Increased overjet.
- Maxillary constriction.
- Generalized spacing between teeth.
- Mandible:
- Retroclination of mandibular teeth.
- Maxilla:
Diagnosis
History
- Family History: Determine the swallow patterns of siblings and parents to check for hereditary factors.
- Medical History: Gather information regarding upper respiratory infections and sucking habits.
- Patient Motivation: Assess the patient’s overall abilities, interests, and motivation for treatment.
Examination
-
Swallowing Assessment:
- Normal Swallowing:
- Lips touch tightly.
- Mandible rises as teeth come together.
- Facial muscles show no marked contraction.
- Abnormal Swallowing:
- Teeth remain apart.
- Lips do not touch.
- Facial muscles show marked contraction.
- Normal Swallowing:
-
Inhibition Test:
- Lightly hold the lower lip with a thumb and finger while the patient is asked to swallow water.
- Normal Swallowing: The patient can swallow normally.
- Abnormal Swallowing: The swallow is inhibited, requiring strong mentalis and lip contraction for mandibular stabilization, leading to water spilling from the mouth.
Management
-
Behavioral Therapy:
- Awareness Training: Educate the patient about the habit and its effects on oral health.
- Positive Reinforcement: Encourage the patient to practice proper swallowing techniques and reward progress.
-
Myofunctional Therapy:
- Involves exercises to improve tongue posture and function, helping to retrain the muscles involved in swallowing and speech.
-
Orthodontic Treatment:
- If malocclusion is present, orthodontic intervention may be necessary to correct the dental alignment and occlusion.
- Appliances such as a palatal crib or tongue thrusting appliances can be used to discourage the habit.
-
Speech Therapy:
- If speech issues are present, working with a speech therapist can help address articulation problems and improve speech clarity.
-
Monitoring and Follow-Up:
- Regular follow-up appointments to monitor progress and make necessary adjustments to the treatment plan.
Anchorage in orthodontics refers to the resistance to unwanted tooth movement during orthodontic treatment. It is a critical concept that helps orthodontists achieve desired tooth movements while preventing adjacent teeth or the entire dental arch from shifting. Proper anchorage is essential for effective treatment planning and execution, especially in complex cases where multiple teeth need to be moved simultaneously.
Types of Anchorage
-
Absolute Anchorage:
- Definition: This type of anchorage prevents any movement of the anchorage unit (the teeth or structures providing support) during treatment.
- Application: Used when significant movement of other teeth is required, such as in cases of molar distalization or when correcting severe malocclusions.
- Methods:
- Temporary Anchorage Devices (TADs): Small screws or plates that are temporarily placed in the bone to provide stable anchorage.
- Extraoral Appliances: Devices like headgear that anchor to the skull or neck to prevent movement of certain teeth.
-
Relative Anchorage:
- Definition: This type allows for some movement of the anchorage unit while still providing enough resistance to achieve the desired tooth movement.
- Application: Commonly used in cases where some teeth need to be moved while others serve as anchors.
- Methods:
- Brackets and Bands: Teeth can be used as anchors, but they may move slightly during treatment.
- Class II or Class III Elastics: These can be used to create a force system that allows for some movement of the anchorage unit.
-
Functional Anchorage:
- Definition: This type utilizes the functional relationships between teeth and the surrounding structures to achieve desired movements.
- Application: Often used in conjunction with functional appliances that guide jaw growth and tooth positioning.
- Methods:
- Functional Appliances: Such as the Herbst or Bionator, which reposition the mandible and influence the growth of the maxilla.
Factors Influencing Anchorage
- Tooth Position: The position and root morphology of the anchorage teeth can affect their ability to resist movement.
- Bone Quality: The density and health of the surrounding bone can influence the effectiveness of anchorage.
- Force Magnitude and Direction: The amount and direction of forces applied during treatment can impact the stability of anchorage.
- Patient Compliance: Adherence to wearing appliances as prescribed is crucial for maintaining effective anchorage.
Clinical Considerations
- Treatment Planning: Proper assessment of anchorage needs is essential during the treatment planning phase. Orthodontists must determine the type of anchorage required based on the specific movements needed.
- Monitoring Progress: Throughout treatment, orthodontists should monitor the anchorage unit to ensure it remains stable and that desired tooth movements are occurring as planned.
- Adjustments: If unwanted movement of the anchorage unit occurs, adjustments may be necessary, such as changing the force system or utilizing additional anchorage methods.
Functional Matrix Hypothesis is a concept in orthodontics and craniofacial biology that explains how the growth and development of the craniofacial complex (including the skull, face, and dental structures) are influenced by functional demands and environmental factors rather than solely by genetic factors. This hypothesis was proposed by Dr. Robert A. K. McNamara and is based on the idea that the functional matrices—such as muscles, soft tissues, and functional activities (like chewing and speaking)—play a crucial role in shaping the skeletal structures.
Concepts of the Functional Matrix Hypothesis
-
Functional Matrices:
- The hypothesis posits that the growth of the craniofacial skeleton
is guided by the functional matrices surrounding it. These matrices
include:
- Muscles: The muscles of mastication, facial expression, and other soft tissues exert forces on the bones, influencing their growth and development.
- Soft Tissues: The presence and tension of soft tissues, such as the lips, cheeks, and tongue, can affect the position and growth of the underlying skeletal structures.
- Functional Activities: Activities such as chewing, swallowing, and speaking create functional demands that influence the growth patterns of the craniofacial complex.
- The hypothesis posits that the growth of the craniofacial skeleton
is guided by the functional matrices surrounding it. These matrices
include:
-
Growth and Development:
- According to the Functional Matrix Hypothesis, the growth of the craniofacial skeleton is not a direct result of genetic programming but is instead a response to the functional demands placed on it. This means that changes in function can lead to changes in growth patterns.
- For example, if a child has a habit of mouth breathing, the lack of proper nasal function can lead to altered growth of the maxilla and mandible, resulting in malocclusion or other dental issues.
-
Orthodontic Implications:
- The Functional Matrix Hypothesis has significant implications for
orthodontic treatment and craniofacial orthopedics. It suggests that:
- Functional Appliances: Orthodontic appliances that modify function (such as functional appliances) can be used to influence the growth of the jaws and improve occlusion.
- Early Intervention: Early orthodontic intervention may be beneficial in guiding the growth of the craniofacial complex, especially in children, to prevent or correct malocclusions.
- Holistic Approach: Treatment should consider not only the teeth and jaws but also the surrounding soft tissues and functional activities.
- The Functional Matrix Hypothesis has significant implications for
orthodontic treatment and craniofacial orthopedics. It suggests that:
-
Clinical Applications:
- The Functional Matrix Hypothesis encourages clinicians to assess the functional aspects of a patient's oral and facial structures when planning treatment. This includes evaluating muscle function, soft tissue relationships, and the impact of habits (such as thumb sucking or mouth breathing) on growth and development.
Growth is the increase in size It may also be defined as the normal change in the amount of living substance. eg. Growth is the quantitative aspect and measures in units of increase per unit of time.
Development
It is the progress towards maturity (Todd). Development may be defined as natural sequential series of events between fertilization of ovum and adult stage.
Maturation
It is a period of stabilization brought by growth and development.
CEPHALOCAUDAL GRADIENT OF GROWTH
This simply means that there is an axis of increased growth extending from the head towards feet. At about 3rd month of intrauterine life the head takes up about 50% of total body length. At this stage cranium is larger relative to face. In contrast the limbs are underdeveloped.
By the time of birth limbs and trunk have grown faster than head and the entire proportion of the body to the head has increased. These processes of growth continue till adult.
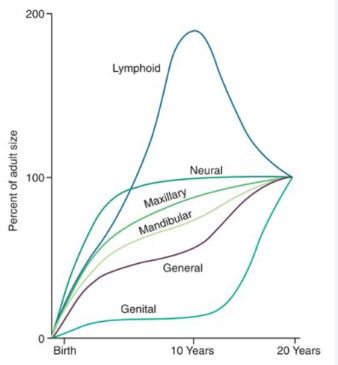
SCAMMON’S CURVE
In normal growth pattern all the tissue system of the body do not growth at the same rate. Scammon’s curve for growth shows 4 major tissue system of the body;
• Neural
• Lymphoid
• General: Bone, viscera, muscle.
• Genital
The graph indicates the growth of the neural tissue is complete by 6-7 year of age. General body tissue show an “S” shaped curve with showing of rate during childhood and acceleration at puberty. Lymphoid tissues proliferate to its maximum in late childhood and undergo involution. At the same time growth of the genital tissue accelerate rapidly.